In mid-December, when news emerged that the number of newborn babies in Japan in 2016 would likely fall below 1 million for the first time since the government started collecting data in 1899, it sparked a renewed debate on how to reverse the downtrend in the fertility rate.
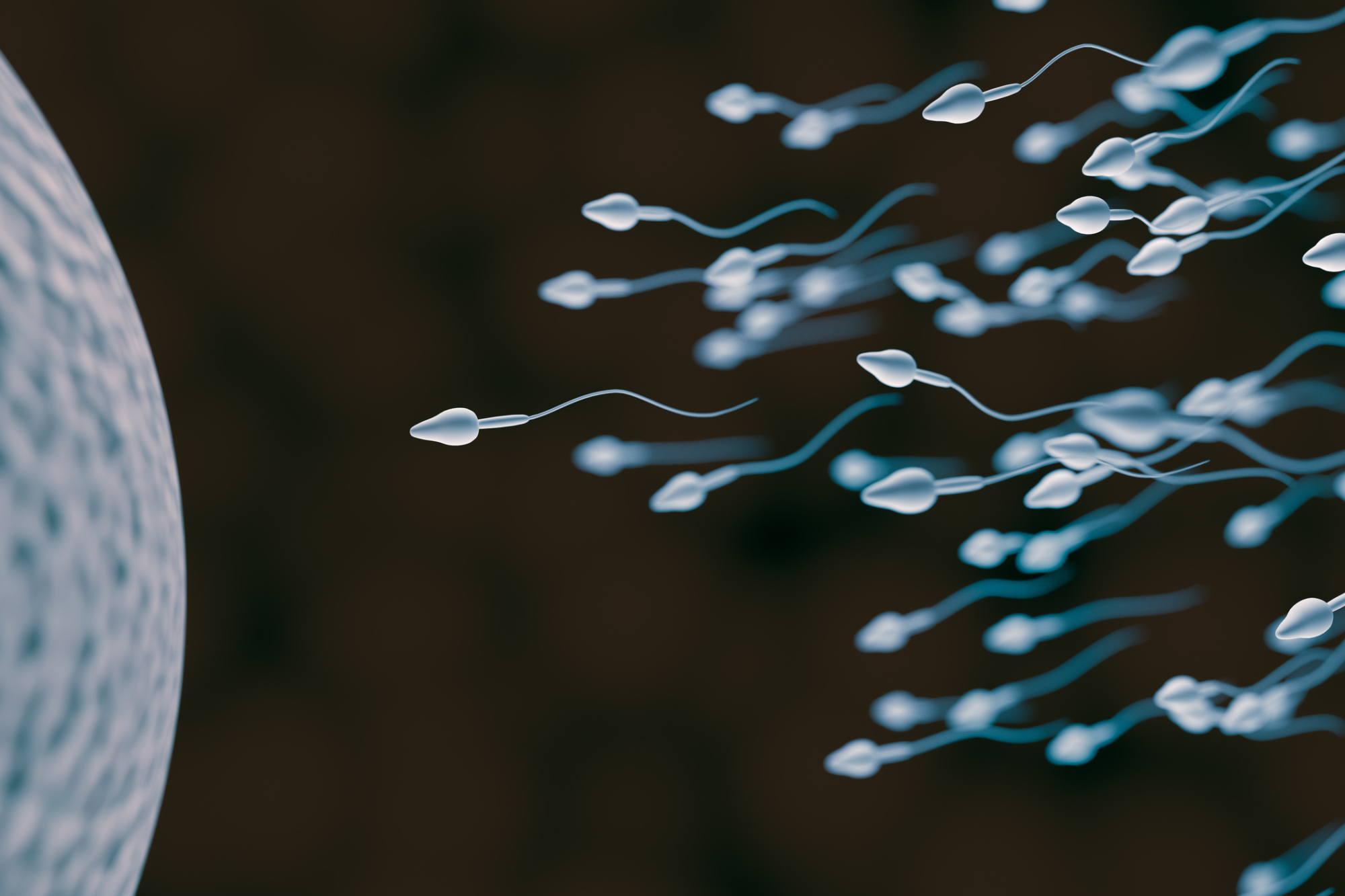
While the usual spade of issues dominated the policy talk — such as increasing state support for child care and reining in excessive overtime to help parental work-life balance — Danish pediatrician Niels E. Skakkebaek had a completely different perspective. For him, the news was a wake-up call for Japan to take a harder look at what has long been ignored and considered taboo: male infertility.
"My main message is that, although we don't know why birthrates are so low, it should be taken into consideration that perhaps poor semen quality contributes to it," Skakkebaek told The Japan Times last month during a visit to Tokyo, where he delivered a lecture at the annual convention of the Japan Pediatric Society. "And that is almost never said in newspapers and other media. They always blame women's work or social factors. But those who work in fertility (treatment) know that infertility is very important."

















With your current subscription plan you can comment on stories. However, before writing your first comment, please create a display name in the Profile section of your subscriber account page.