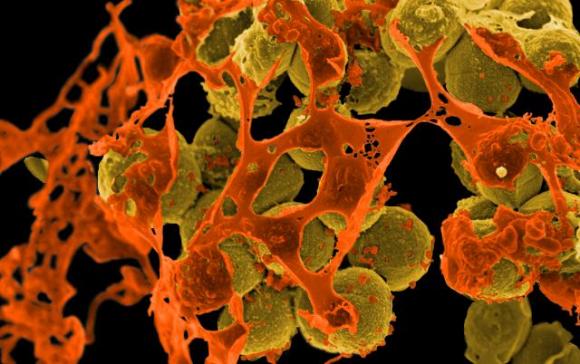
Public health officials have begun tackling the misuse and overuse of antibiotics, as the prevalence of superbugs, or bacteria resistant to antibiotics, reaches alarming levels worldwide.
A panel of experts under the Health, Labor and Welfare Ministry on Monday adopted draft guidelines on when doctors should refrain from using antibiotics. These guidelines, soon to be finalized and distributed to clinics and hospitals across the nation, explicitly discourage prescribing antibiotics to treat common colds or acute diarrhea.
For years, doctors have dispensed antibiotics for minor ailments, such as a sore throat or fever, even though the drugs, which are meant to kill or inhibit the growth of bacteria in the body, have little effect on colds or other viral illnesses.

















With your current subscription plan you can comment on stories. However, before writing your first comment, please create a display name in the Profile section of your subscriber account page.