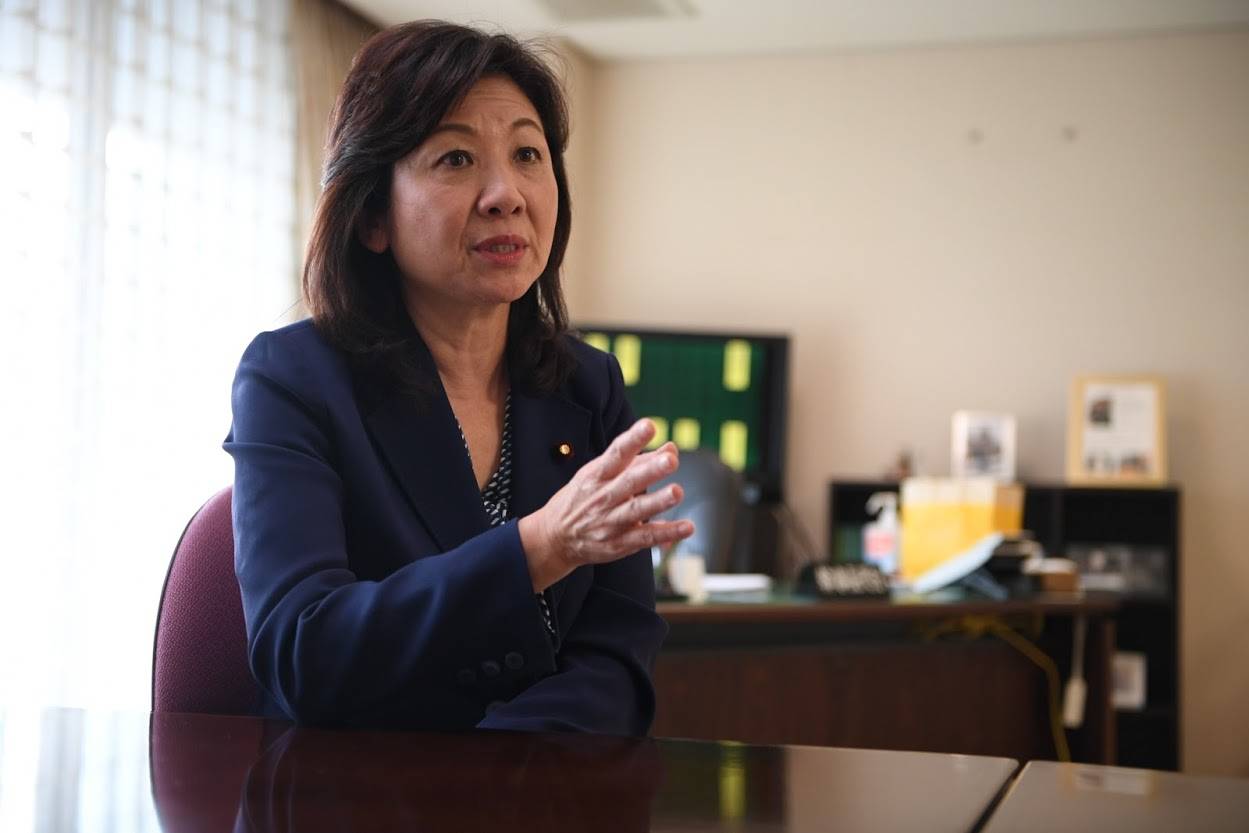
In 2010, one of Japan’s most prominent female politicians, Seiko Noda, sparked controversy by bearing a child at age 50 through artificial insemination after years of infertility treatment.
“What bothered me is that especially in the initial stage (of the therapy), I wasn’t even able to say it out loud that I was going through (infertility treatment) and I felt as if I were doing something you just don’t tell people about,” she said while looking back on the push to improve infertility care in Japan.
Although infertility treatment options and access to such care in Japan have expanded over the years, the stigma associated with infertility has for decades made women keep their struggles under wraps. Ten years after Noda's own experience, the government is eyeing health reforms, primarily aimed at reducing the cost of infertility treatment using more advanced reproductive techniques, as early as April 2022. But the veteran lawmaker believes that easing financial burdens will not be enough to help women in pursuit of motherhood raise their chances to conceive.
















With your current subscription plan you can comment on stories. However, before writing your first comment, please create a display name in the Profile section of your subscriber account page.