October is Pink Ribbon Month: an annual campaign to increase awareness about breast cancer and get more women screened in order to catch the disease in its early stages, which will boost survival rates.
And as part of the campaign, buildings are lit up in pink and cancer survivors and doctors hold lectures nationwide to get the message out.
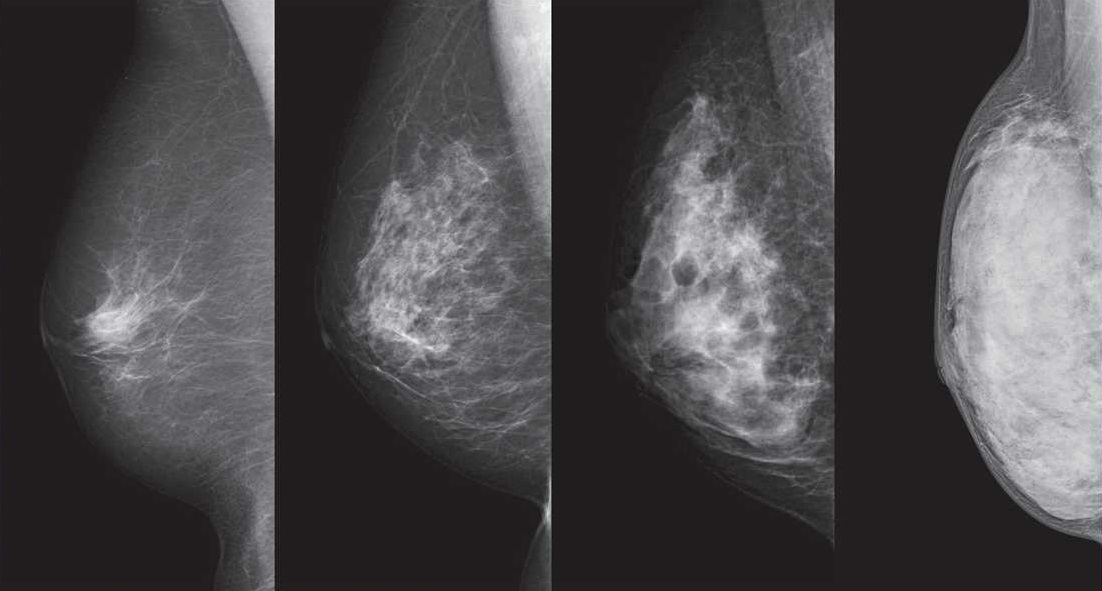
But experts in Japan remain divided — and undecided — on one issue surrounding breast cancer screenings and that is whether to tell people who undergo the tests if they have dense breast tissue.















With your current subscription plan you can comment on stories. However, before writing your first comment, please create a display name in the Profile section of your subscriber account page.