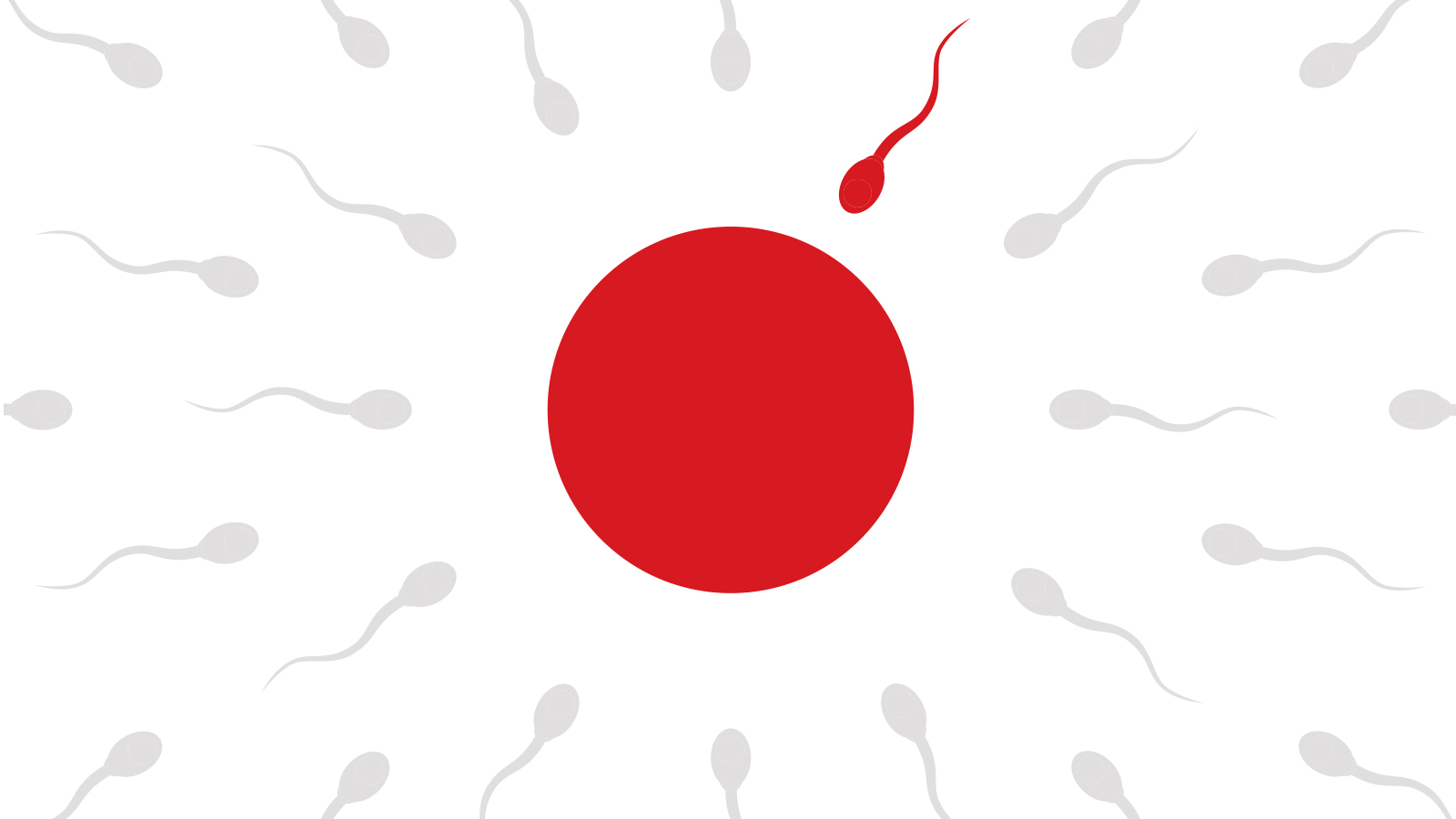
One out of 27 children in Japan today are born through in vitro fertilization. More astonishingly, 1 out of 6 couples suffer from infertility. With about 600 fertility clinics and hospitals in operation nationwide, Japan has become known as something of a "superpower of fertility treatment."
With more and more people starting to have children later in life, an increasing number of couples are turning to medical support to conceive.
What was once an issue that was rarely discussed because of the social stigma attached to it, fertility treatment has become such a common procedure that people are more willing to consider it without hesitation.