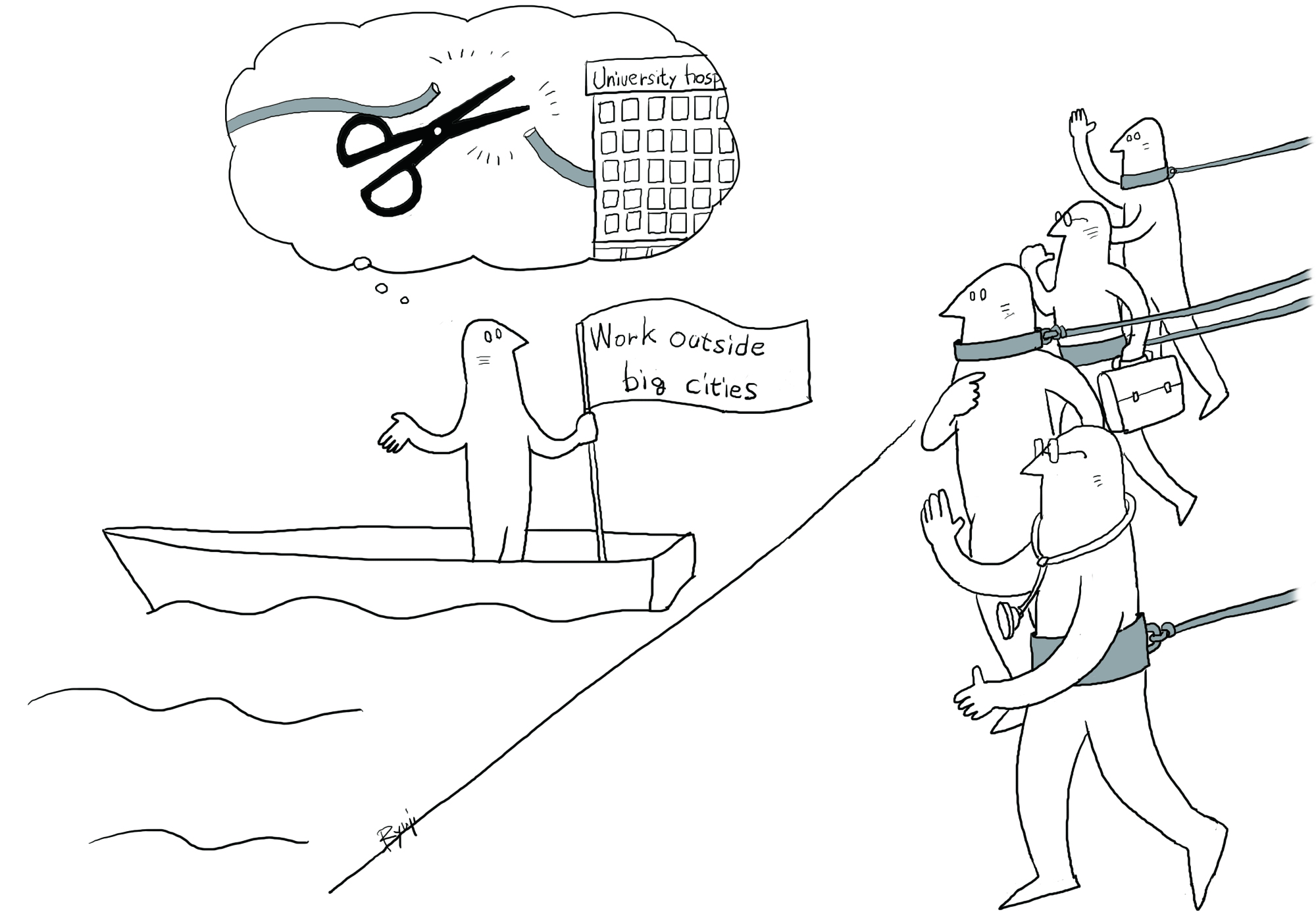
There has long been a widespread myth that medical doctors in general prefer not to leave big cities, causing a shortage of physicians in rural parts of the country and the resulting poor medical services accelerating depopulation. This myth has been proved false by a study undertaken by the Health, Labor and Welfare Ministry. But it is the ministry itself that has colluded with university hospitals in major cities to spread this false view in order to protect their vested interests. The study, initiated by health minister Yasuhisa Shiozaki, has exposed an "inconvenient truth" that the ministry did not want publicized.
There is no denying that rural regions of Japan face a serious shortage of doctors. In February, the Iwaki Kyoritsu Hospital run by the municipal government in Iwaki, Fukushima Prefecture, stopped accepting hospitalization of pulmonary tuberculosis patients when no replacement could be found for a full-time pulmonologist who reached mandatory retirement age. Iwaki, population 340,000, now has no full-time doctor to treat respiratory patients. In March, the Tarumizu Tokusuikai Hospital in Tarumizu, Kagoshima Prefecture, closed partly because it could not secure enough doctors. The shutdown of a hospital belonging to the nationwide Tokushukai group in its home turf came as a shock in medical circles.
The annual number of hospitals and clinics that were shut down or dissolved shot up from 121 in 2007 to 347 in 2014. The health ministry attributed this to what it described as a tendency among young doctors to prefer working in metropolitan areas and avoid working outside of big cities. It is ironic that the ministry's own study has proved this assertion to be totally false.