Aimee Robeson just wants an answer.
Her son, Christian, was born in 2010 with multiple mysterious syndromes that leave him unable to speak, chew or walk on his own.
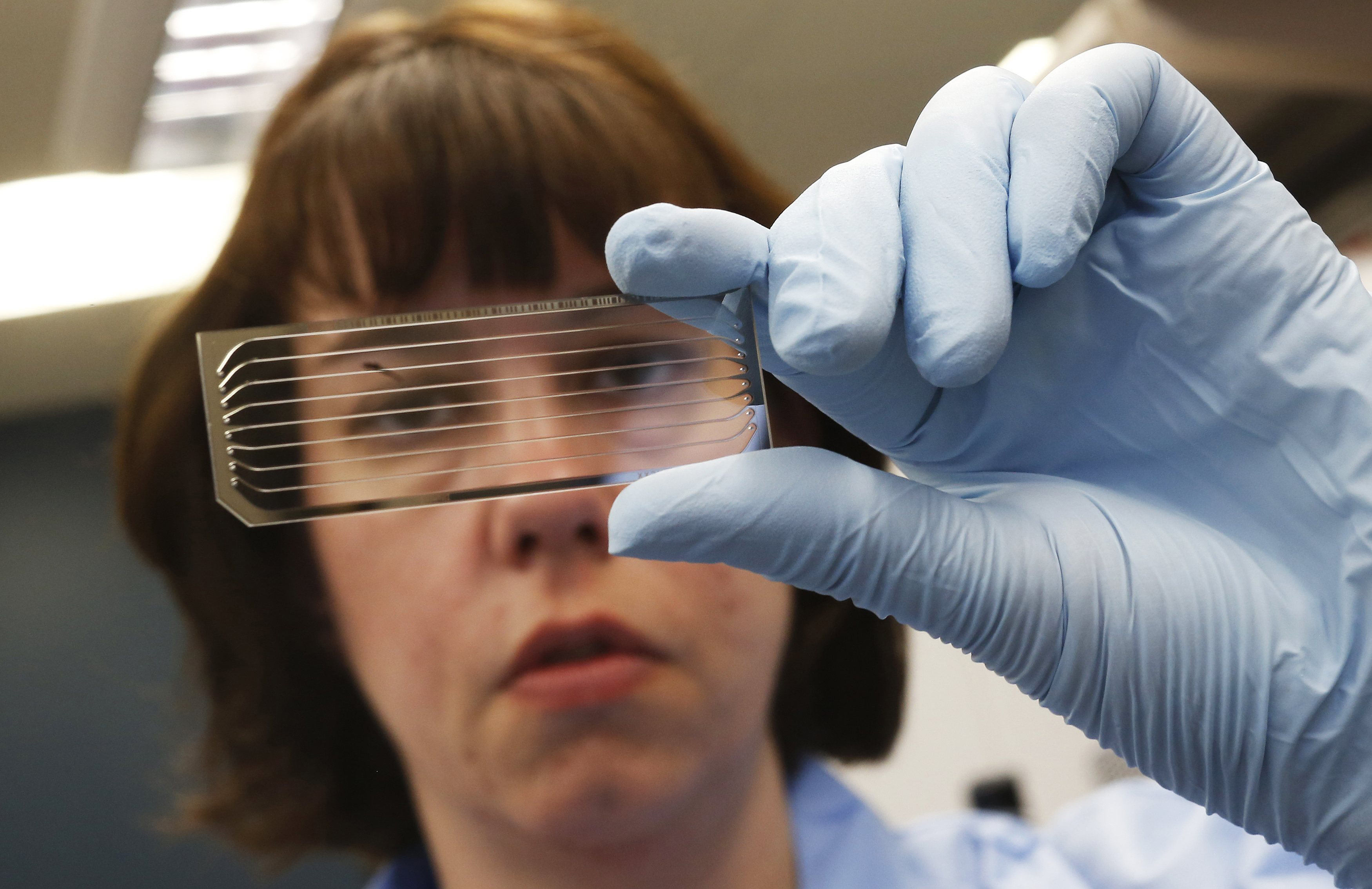
Initial genetic tests failed to provide a diagnosis. Aimee's hopes are now pinned on a new test called exome sequencing that searches all the protein-making genes for glitches that could explain her son's condition.